Reston/Herndon - (703) 437-6333
Manassas/Gainesville - (703) 368-7166
-
Innovations in Foot and Ankle Surgery
posted: Feb. 15, 2024.
-
Choosing the Right Foot Doctor
posted: Dec. 08, 2023.

-
How To Prevent Bunions
posted: Nov. 07, 2023.

-
What Problems Do Podiatrists Treat?
posted: Jul. 03, 2023.
If you are dealing with heel pain, bunions, ingrown toenails, or other issues affecting your feet or ankles, a foot doctor can help. Podiatrists diagnose and treat all types of Read more -
What Causes a Bunion?
posted: Jun. 02, 2023.
Seek the help of our podiatrists at Reston & Manassas Foot and Ankle Centers if you need bunion treatment in Manassas & Reston, VA. How Do You End Up With a Read more -
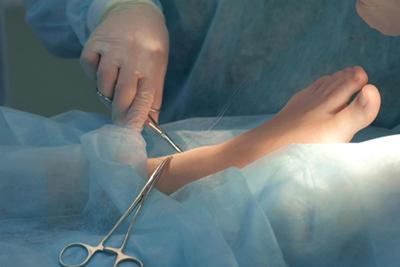
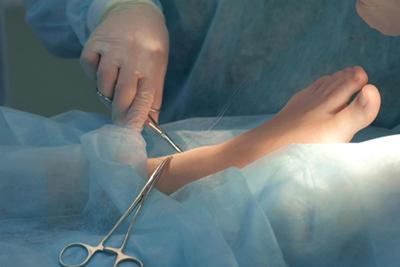
What To Expect During Your Foot or Ankle Surgery
posted: Feb. 27, 2023.
Your foot and ankle are complex and there are many issues that might impact you. When you’re dealing with different types of foot and ankle issues, the best option might Read more -
Treating Heel Pain
posted: Dec. 16, 2022.
The podiatrists at Reston, Manassas, and Leesburg Foot and Ankle Centers in Reston, Manassas, and Leesburg, VA, can help your heel pain whether you've been suffering from this ailment for Read more -
Suffering From Heel Pain?
posted: Oct. 26, 2022.
Find out when to turn to our foot and ankle team for care. Heel pain can often be treated with home care, but what happens when your heel pain isn’t responsive Read more -
When to See a Podiatrist
posted: Aug. 16, 2022.
When your feet hurt, it can seriously impact your mobility. Sore feet can happen at any age and can be caused by many things. If you need a podiatrist in Manassas Read more -
When to Visit Your Podiatrist
posted: Aug. 09, 2022.
Your feet are an incredibly important part of the body and are necessary for most daily functions. When you start experiencing foot pain, it can be frustrating to deal with Read more -
What To Do When You Have Heel Pain
posted: Jun. 10, 2022.
How your podiatrists in Reston, Manassas, and Leesburg, VA, can help you get relief from heel pain If you suffer from heel pain, you already know how it can impact your Read more -
Treatment Options For Bunions
posted: Mar. 29, 2022.
When you have arch problems or wear shoes that don’t fit properly, you’re at risk for developing bunions. Bunions are a hard, bony knob that appears on the side of Read more -
What Does a Foot Doctor Treat?
posted: Feb. 10, 2022.
At Reston, Manassas, and Leesburg Foot and Ankle Centers, our team of skilled podiatrists is ready to become your go-to foot doctor in Manassas & Reston, VA, and Leesburg, VA. Read more -
When Should I Be Concerned About Heel Pain?
posted: Jan. 11, 2022.
Your podiatrists in Reston, Manassas, and Leesburg, VA, can help you get relief from heel pain If you have heel pain, you may be waiting for it to go away on Read more -
Can You Heal a Bunion Without Surgery?
posted: Dec. 08, 2021.
Bunions are a bony projection that will sometimes form on the inside of your foot at the joint where the big toe meets the foot. Once a bunion has progressed to a Read more -
When You Should Visit a Foot & Ankle Surgeon
posted: Nov. 11, 2021.
Reston, Manassas, and Leesburg Foot and Ankle Centers is accepting new patients and has a staff that is ready to help patients with any questions or concerns regarding injuries they Read more
Contact Us
Send Us An Email
Contact Us
Locations
Reston Foot and Ankle Center
1760 Reston Pkwy, Suite 310
Reston, VA 20190
Phone (703) 437-6333
Fax: (703) 437-7837
Manassas Foot and Ankle Center
8577A Sudley Rd.
Manassas, VA 20110
Phone (703) 368-7166
Fax: (703) 368-5103
Office Hours
Reston Foot and Ankle Center
Monday - Thursday: 9:00am - 5:00pm
Friday: 9:00am - 3:00pm
Manassas Foot and Ankle Center
Monday - Thursday: 9:00am - 5:00pm
Friday: 9:00am - 3:00pm
